Menopause is a stage in a woman’s life when her menstrual cycles stop and she loses the ability to have children forever. During this time, a variety of physiological and psychological symptoms can occur. Research indicates that cannabis can alleviate some of these symptoms.
More specifically, menopause is defined as the absence of a woman’s menstrual cycles for 12 months; the periods of biological change before and after this point are called “perimenopause.”
The endocannabinoid system plays a key role in all aspects of female fertility, from initial fecundity to implantation of the developing embryo into the endometrium and transmission of endocannabinoids through breast milk. The endocannabinoid system also has a critical function in terminating fertility.
What is menopause?
During perimenopause, women usually begin to have irregular menstrual cycles and hormone levels begin to fluctuate.
During postmenopause (the years after menopause), women generally have lower levels of reproductive hormones and are more prone to urinary tract infections, weight gain, and various other health complications.
Symptoms of perimenopause
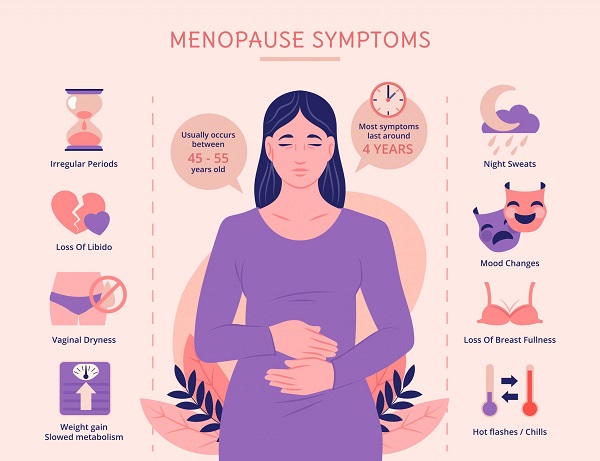
During perimenopause, which usually occurs between the ages of 45 and 55, various unpleasant and sometimes debilitating symptoms occur. These symptoms can be divided into three types: vaginal/uterine, other physical and psychological.
-
Vaginal/uterine symptoms include vaginal dryness, pain during intercourse, and atrophic vaginitis (a condition in which the mucous membranes of the vagina, vulva, and related tissues become thin and lose elasticity).
-
Other physical symptoms include night sweats, palpitations, dizziness, headaches, stiffness, back pain, chest pain, urinary incontinence, night sweats, insomnia and hot flashes.
-
Psychological symptoms include anxiety, depression, loss of attention, memory problems, mood swings, and loss of libido.
Effects of the Endocannabinoid System on Menopause

Unfortunately, to date, there are only sporadic studies examining the complex role of the endocannabinoid system in female fertility in general, including the onset of menopause. According to these studies, a variety of significant changes in the endocannabinoid system and related biological processes occur during the transition to menopause.
Menopause is associated with an increased risk of osteoporosis, which is thought to be related to changes in the functioning of the endocannabinoid system in bone structure (https://my.clevelandclinic.org/health/articles/10091-menopause–osteoporosis). A 2011 study found that postmenopausal women diagnosed with osteoporosis have overexpression of CB2 receptors in osteoclasts (the cells responsible for bone resorption), which causes overactivity of osteoclasts and leads to excessively rapid bone resorption (http://www.thebonejournal.com/article/S8756-3282(11)00002-0/abstract).
Menopause also affects the body’s insulin sensitivity and may increase insulin resistance (which, in turn, may contribute to the development of type 2 diabetes) in some postmenopausal women (europepmc.org/abstract/med/8405521). Moreover, a 2013 Canadian study found that obese postmenopausal women who experienced insulin resistance also had higher levels of circulating endocannabinoid 2-AG in their blood, reduced levels of anandamide, and increased CB1 receptor activity compared with individuals who maintained insulin sensitivity (https://onlinelibrary.wiley.com/doi/full/10.1002/oby.20498).
The relationship between the endocannabinoid system, the transition to menopause, and the risk of weight gain requires further study. An earlier study in 2005 in Germany showed that postmenopausal women with obesity had significant increases in both anandamide and 2-AG compared to participants without obesity (http://diabetes.diabetesjournals.org/content/54/10/2838.full). A similar decrease in the FAAH enzyme responsible for the breakdown of endocannabinoids was also seen in obese women.
Genetics, menopause and ECS

There are also genetic factors that regulate the function of the endocannabinoid system at key stages of the female reproductive cycle. Studies indicate that people with certain single-nucleotide polymorphisms (SNPs) have different physical responses to menopause, depending on how the ECS system functions.
A 2011 study by the same Polish research team found that another SNP, RS2023239 of the CNR1 gene, may be associated with an increased “free androgen index” in postmenopausal women who have it (http://informahealthcare.com/doi/abs/10.3109/09513590.2011.569796). In turn, elevated levels of free androgens (male reproductive hormones such as testosterone) may be associated with an increased risk of cardiovascular disease.
How does cannabis help menopausal women?
Osteoporosis
CB2 receptors of osteoclasts are mainly involved in the development of osteoporosis. The SNPs in the CNR2 gene responsible for CB2 receptor expression have been found to be closely associated with the occurrence of osteoporosis in postmenopausal women (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3001217/).
In addition, it is now known that CB1 receptors also influence the development of osteoporosis. A 2005 study in mice with deactivated CB1 receptors demonstrated increased bone mass and protection against ovariectomy-induced bone loss (http://www.ncbi.nlm.nih.gov/pubmed/15908955/). Several studies have also shown that CB2 receptor antagonists reduce bone mass loss. Thus, CB receptor deactivation appears to be a key factor in reducing the excessive rate of bone resorption leading to osteoporosis.
Weight gain
Although there are limited studies of altered ECS function in postmenopausal obese women, there are currently no specific studies confirming the ability of cannabinoids to control or reverse weight gain in such cases. In general, however, CB receptor blockers may contribute to weight gain.
Several studies have shown that the synthetic, selective reverse CB1 receptor agonist rimonabant, is capable of inducing weight loss in humans. However, this drug has been taken off the market because of the potential for serious psychiatric side effects, including suicidal ideation.
However, the prevalence of obesity among cannabis users is much lower than in the general population, which may be due to the synergistic effects of THC combined with CBD. Thus, non-synthetic medical cannabis may be just as (if not more) effective than any synthetic cannabinoid and have far fewer potential side effects.
Insomnia
While there are no specific studies supporting the ability of cannabis to help menopausal women with insomnia, there are scientific papers that support the effectiveness of various cannabinoids in this matter. For example, anandamide and the THC analogue marinol may speed up falling asleep, improve sleep quality and reduce the likelihood of waking during sleep, according to a 2007 review (http://onlinelibrary.wiley.com/doi/10.1002/cbdv.200790150/abstract). In addition, CBD products may also be helpful, as studies show that they can increase overall sleep time (https://journals.sagepub.com/doi/abs/10.1177/0269881112474524).
Insulin Resistance
Several studies have been conducted to examine the relationship between the endocannabinoid system, insulin resistance, and the development of diabetes (http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0005844). According to these studies, CB-receptor blockers play an important role in controlling insulin resistance. This is supported by the fact that CB2 knockout mice show reduced insulin resistance, while CB1 receptor blockers have been shown in multiple studies to reduce diet-induced insulin resistance.
Pain syndrome
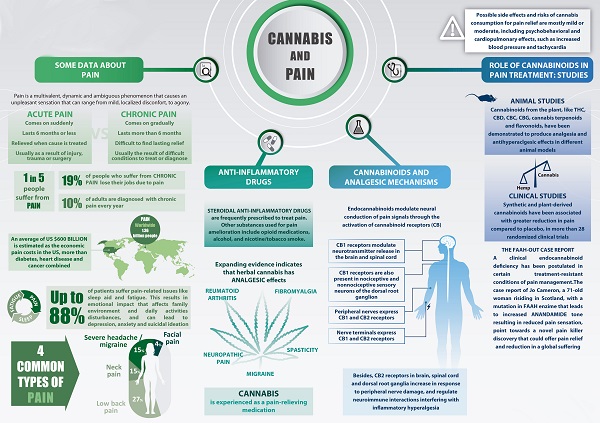
Over the past decades, there have been many studies on the ability of THC to manage pain. The general consensus among scientists is that CB receptor agonists are more effective than blockers in treating pain (http://www.pnas.org/content/96/21/12198.short).
Studies have shown that CB1 and CB2 receptors (THC, AM1241, anandamide, and so on), have antinociceptive effects in cases of chronic pain (https://www.sciencedirect.com/science/article/pii/S001502820102934X). During menopause, inflammation often becomes an issue due to decreased estrogen levels, which can lead to pain. Cannabidiol (CBD) has anti-inflammatory properties, so it may be useful for pain related to inflammation during menopause (https://www.ncbi.nlm.nih.gov/pubmed/22585736).
Anxiety
The role of the endocannabinoid system in mediating anxiety remains somewhat controversial and is probably dose dependent. Low doses of CB receptor agonists appear to cause anxiolytic effects, whereas high doses may have the opposite effect. In addition, inactivation or deletion of the CB1 receptor appears to cause anxiogenic effects (link.springer.com/chapter/10.1007%2F7854_2009_16#page-1).
Loss of libido
Studies have shown that THC and the reverse CB1 receptor agonist AM251 increase sexual motivation and receptivity in female rats, indicating a possible role for CB1 receptor blockers in the treatment of libido loss in women (www.sciencedirect.com/science/article/pii/S009130570800347X).
In addition, CBD may also help in this case.
Estrogen plays an important role in stimulating blood flow to a woman’s vagina by helping with lubrication (https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1038/sj.bjp.0706687). When estrogen levels drop, this can become a problem. CBD is a powerful vasodilator that can help increase blood flow.
Some restrictions

Cannabis certainly causes xerostomia (dry mouth). In the popular press, THC use is also often linked to vaginal dryness, but there is not really enough evidence for such a claim. A 2009 study called Cannabis and Sexual Health provided the basis for this link, but upon closer examination it becomes apparent that the link between cannabis use and vaginal dryness was in fact too weak to achieve statistical significance.
Furthermore, the mechanism underlying the formation of vaginal lubrication is quite different from that of salivation.
However, there is evidence that cannabis can actually increase sexual arousal, which is likely to have beneficial effects on the natural processes of vaginal lubrication.
Some evidence suggests that cannabis can cause acute cardiovascular events in susceptible people . It seems that agonists such as THC are more likely to be involved in such events, and therefore it may be advisable to avoid THC if you suffer from palpitations. This is especially true if there is a risk of any pre-existing condition.
In general, it seems that CB receptor blockers may be useful as an adjunctive treatment for menopause-related disorders, including osteoporosis, weight gain, and loss of libido, while agonists such as THC may be useful in treating pain, anxiety, and insomnia.